Mycetoma
Virtual Doctors Work
As we move from Summer to Autumn in the UK and we see rain causing so much disruption and devastation around the world, I wondered about the effects of the changing seasons on health in Zambia. Situated in the tropics, Zambia gets lots of strong sunlight, but the intense heat that comes in the tropics is moderated here by the altitude and rainfall. There are two main seasons in Zambia, the rainy season (November to April), and the dry season (May to October/November). The dry season is divided into a cool and a hot time. The rainy and dry seasons are clearly distinct- with no rain falling at all in June, July and August (usually) followed by hot, wet downpours. Much of life is dominated by the start and end of the rainy season or ‘emerald season’ as it is known and the amount of water it brings. Failure of the rains to come can cause famine. The highest rainfall is in the north with the driest areas in the far southwest and the Luangwa River. Rainfall varies over a range of 500- 1400mm per year.
Flooding occurs every year on the floodplains. Those living in these areas, both people and wildlife, are well adapted to cope with this. However untarred roads become quagmires, many completely impassable. Rivers swell and burst their banks washing away trees, roads and bridges. Many rural areas can be cut off for a few months, making getting anywhere away from the main routes very difficult!
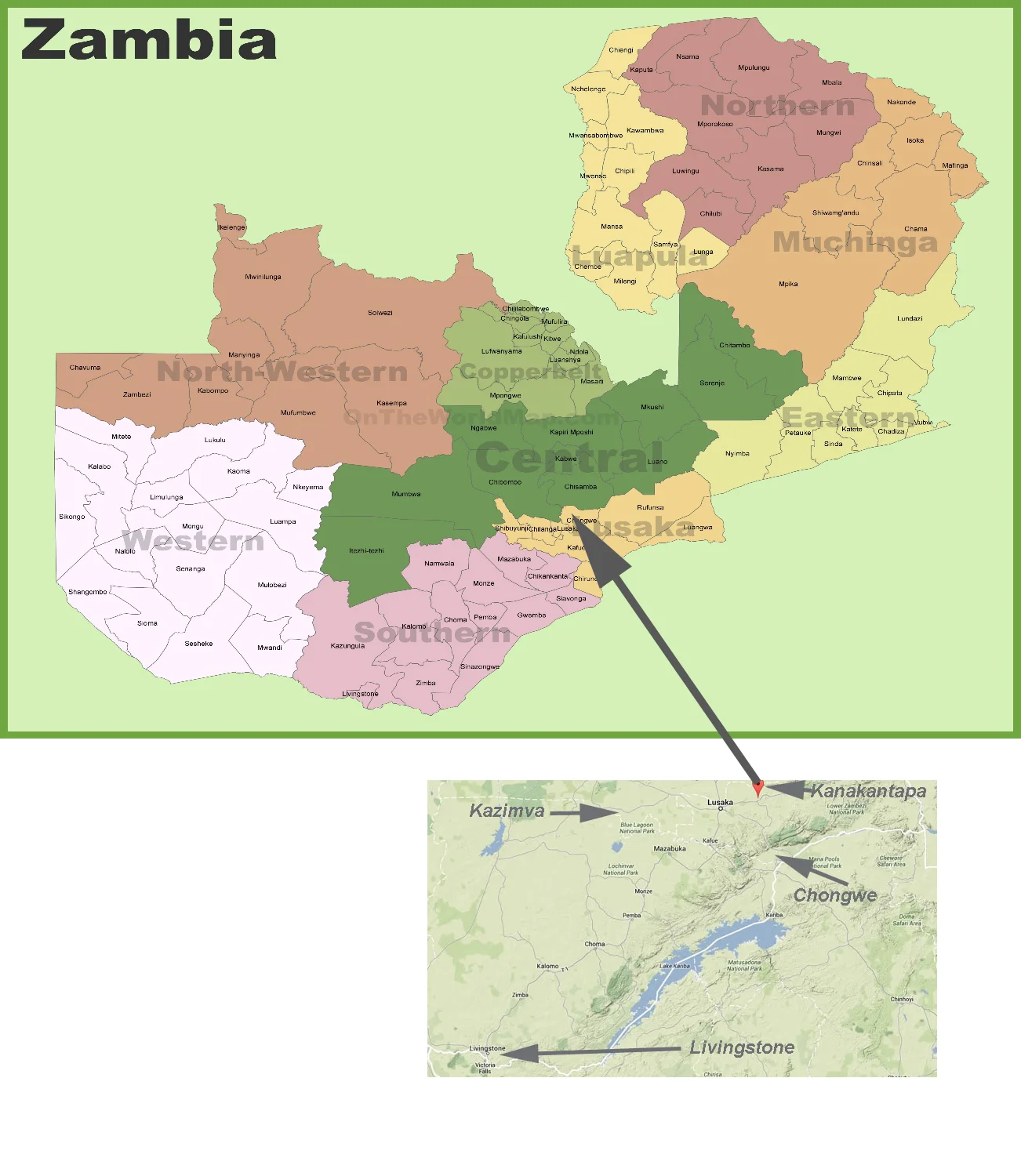
For this month’s case we return again to the Lusaka province which sits on the Zambezi flood plains. This time to Kanakantapa Rural District Health Centre in Chongwe district. Kanakantapa Rural Health Centre serves over 13,000 people from the surrounding communities which are predominantly farming areas. The Kanakantapa river lies to the west of Kanakantapa. It is crossable in the dry season but during the rainy season when the water levels rise and as there is no bridge it becomes impassable, increasing the distance to get to Chongwe by 5 km.
Lusaka Province showing Chongwe distict
Within Chongwe district we support 2 rural health centre and the district hospital.
The difficulties travelling to Kanakantapa clinic after a downpour.
Kanakantapa Rural Health centre
To the clinic, a mother brought her 2 year 11 month old boy to be seen. He is suffering from sores on his feet which have a watery discharge. These sores apparently often return during the rainy season. The clinical officer (CO) had seen quite a few cases like this and was struggling to treat them. For this child he had tried 2 courses of antibiotics; one oral and the next intramuscular (injection into the muscle) with no improvement. The CO included some good quality photos. These are so helpful in skin cases.
The Virtual Doctor (VDr) wasn’t entirely sure what the diagnosis was. But, as it was a particular rainy season problem and antibiotics hadn’t worked, thought it was likely to be a fungal infection. She advised starting some antifugal medicine by mouth. The advice was gratefully received although the clinic had limited supplies so the CO would have to order some medication to be sent. Tricky in the rainy season.
Meanwhile the VDr asked for a second opinion from a dermatologist in the UK. This condition is something not seen in the UK. The dermatologist thought that is was most likely to be Mycetoma. Advice was for further investigation to distinguish between a bacterial and fungal cause of the infection.This could be done by taking a potassium hydroxide slide of the discharge and seeing if fungal elements or filamentous bacteria could be seen under a microscope. A relatively low tech investigation to perform. And then to treat with antifungal medication if fungus was seen. The nails on the patient’s left foot looked abnormal (dystrophic), suggesting a fungal infection. The dermatologist suggested trying treatment but noted that the response to treatment in this infection is generally poor.
What is Mycetoma?
Mycetoma is an uncommon chronic, infective skin and subcutaneous (tissues beneath the skin) disease. It presents with painless lumps under the skin, starting small they can grow, break down and form sores which ooze pus. It can cause the affected limb to become deformed or unusable. If left untreated or treatment fails, it can spread to other areas of the body. Sometimes surgery is needed to cut away infected tissue. Long- term it can destroy underlying muscle and bone. It most commonly affects the foot and it is also known as ‘Madura foot’ after the Indian region where it was first described in 1842. It is a health problem in equatorial regions of Africa, Latin America and Asia known as the ‘mycetoma belt’.
What Causes Mycetoma?
The source of this infection is found in the soil and water and is caused by certain types of both bacteria and fungi. It is likely they enter the body through breaks in the skin. Typically it presents in agricultural workers or those who walk barefoot. It develops over time as it requires repeated exposure of broken skin to the soil and water that contains the microbes. Fungal mycetoma (eumycetoma) is the most common type in Africa. Mycetoma does not spread between people.
Diagnosis and Treatment.
Mycetoma is best diagnosed by taking a small sample (biopsy) of the affected area of the body or the discharge and examined under a microscope to help determine if the infection is caused by bacteria or fungi. Cultures (growing the bacteria or fungi in a laboratory) from the discharge or biopsy can determine the specific type of microbe. Further imaging maybe needed to see how much damage to underlying muscle and bone has occurred.
Treatment depends on whether it is a bacterial or fungal cause:
Bacterial or Actinomycetomais usually treated with antibiotics and surgery generally not required.
Fungal or Eumycetoma is treated with long term anti-fungal medication, but sadly treatment may not be completely effective. If this is the case then surgery or amputation are sometimes needed.
So early diagnosis and treatment is vitally important and wearing shoes might help to prevent Mycetoma.
Disclaimer: This article is for information only and shouldn’t be used for diagnosis or treatment of medical conditions. If you have any concerns about your health consult a doctor or other health professional.