Bells Palsy and TMJ Dislocation
Telemedicine is certainly challenging, as many UK Doctors have discovered over recent months. Much of the Art of Medicine relies upon direct Patient-Doctor interaction; being able to tell immediately ‘from the end of the bed’ that someone is acutely unwell, understanding a patient’s concerns through non-verbal communication, eliciting clinical signs using expert examination skills and so on. Moving consultations to phone or screen might risk losing some of the vital benefits of real face-to-face interactions.
At Virtual Doctors we aim to use Digital health to share our clinical skills. As a Volunteer it can be difficult at first to adapt to our model of remote consultation. But with our Telemedicine system we have a Clinician on site who is face-to-face with the patient. They are practising the Art of Medicine for us. We rely on the Clinical Officers to gather all the relevant information and to look for clinical clues on examination. Together we can then formulate an appropriate management plan for the patient. With ongoing feedback and education we aim to optimise the skills of local clinicians, not just with the aim of facilitating effective referrals but with the goal of empowering them and improving patient care.
Below we share two cases where the Clinical Officers were able to provide a clear description of the patient’s problem; they used our Telemedicine service to help them make sense of their findings and to understand the next steps in management.
credit Adam Hoglund/Shutterstock.com
BELL’S PALSY
A 31-year old male presented with a 24-hour history of weakness affecting the right side of his face. The question was, had this had been caused by a stroke?
Helpfully, the Clinical Officer reported that the patient was not suffering from weakness of his arms or legs and had no speech or visual disturbance. But he was unable to close his right eye and his mouth was drooping. When he tried to raise his eyebrows there was clear weakness affecting the whole of the right side of his face, with loss of forehead wrinkling. This is an important sign and, together with the absence of other neurological symptoms, suggested that the weakness was not due to a stroke (where the forehead is ‘spared’ and still able to wrinkle) but instead due to a lower motor neurone facial nerve palsy.
Yogesh B Gavali/Shutterstock.com
The Volunteer suggested checking around the ears for the typical blisters of Herpes Zoster (a virus) that can sometimes cause weakness of the facial nerve. No rash was found. Many cases of this kind of facial nerve palsy are idiopathic (or of unknown cause) and we call this a “Bell’s Palsy”.
Steroids can help speed up recovery if started early after symptom onset. Our Doctor recommended a 10-day course. They explained the dosing regimen and the possible side effects of treatment to look out for. Importantly they also passed on tips for eye care. The patient was unable to close his eye properly and there was a risk it would become dry, irritated and damaged. Lubricating eye drops and wearing an eye patch can help.
The Volunteer shared a link to useful guidelines about this condition and also offered to send information about exercises the patient could do to help regain strength in the facial muscles. They suggested that the patient was made aware of the possibility that, whilst most people make a full recovery, others are left with persistent problems.
The patient was very grateful to have been managed locally at the clinic without having to make a long trip to hospital. We were pleased to hear that when he returned for review several weeks later there was already an improvement in his symptoms.
TEMPOROMANDIBULAR JOINT DISLOCATION
A 37-year old lady presented to Kalomo saying she could not close her mouth. This was causing her significant discomfort. She described how her symptoms started suddenly after yawning several hours earlier. She was finding it difficult to move her mouth and couldn’t speak clearly.
She was otherwise well. She had no past medical history of note and was not on any medications.
On examination she appeared distressed. Her mouth was held open and the jaw was sticking out and to the right. She was drooling saliva. There were no other abnormalities.
From the information provided it sounded as though this lady had temporomandibular joint dislocation. This happens when the bony condyle of the jaw moves forward and then becomes stuck, preventing closure of the mouth. This can happen after the mouth has been opened wide (e.g. during eating, yawning, laughing, vomiting and dental treatment etc.). It can also be seen as a consequence of seizures, dystonic drug reactions or tetanus infection. Patients with certain connective tissue diseases may be predisposed to this condition because there is weakness of the joint capsule. Most commonly bilateral dislocation occurs but it can be one-sided and result in the jaw deviating towards the unaffected side, as in this patient.
It can be very painful, and the patient may experience discomfort in the temporal region (on the side of the forehead) or in front of the ear, as well as in the jaw itself. The Volunteer suggested that the priority was to ensure that the patient had adequate analgesia. In addition, an agent to help relax the muscles is helpful.
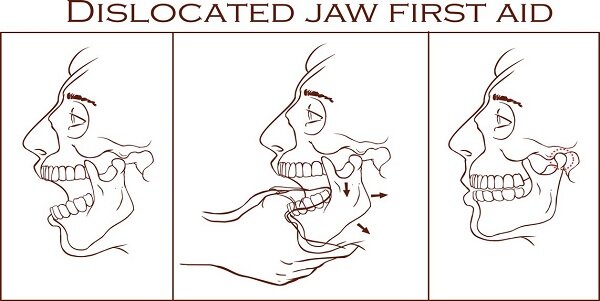
The aim is then to try and reduce the dislocation; the sooner the better, otherwise it becomes more difficult. The Volunteer highlighted to the Clinical Officer that manual reduction should not be attempted if there is a history of trauma as there may be an underlying jaw fracture and you may cause harm; these patients would need X-rays first. In this lady’s case it sounded as though it had been the yawning that caused the dislocation and so it was appropriate to attempt reduction on site.
credit Corbac40/Shutterstock.com
There are various techniques for reducing the dislocation and the Volunteer described one of these to the Clinical Officer (as well as sharing a link to an online clinical video of the procedure). In essence the jaw can be relocated with pressure applied to the molar teeth and lifting of the chin. The Doctor shared tips for a successful procedure; waiting for the medication to take effect before starting, positioning the patient properly and not rushing the manoeuvre.
In this case the reduction was successful, and the client was profoundly grateful to the Clinical Officer! We are told she thanked him ‘like a God’! The Virtual Doctor advised that if all was well she could return home, with adequate analgesia to take away. It was recommended that she have a soft diet for a few days until things had settled down. The patient was very happy that her problem had been managed so swiftly on site as she was instantly more comfortable; the Clinical Officer was glad that there had been no delay as travel to another centre may ultimately have resulted in a more difficult procedure.
Even though the Doctors involved in these cases were at a distance, they were confident in their diagnoses. There was a Clinician face-to-face with the patient to ensure that the appropriate management plan was enacted swiftly. Both cases had a good outcome and the Clinical Officers felt they had gained valuable experience for the future.