Complications in pregnancy
INTRODUCTION
The WHO estimates that more than 800 women die every day from preventable causes related to pregnancy and childbirth. Around two-thirds of these deaths (almost 200,000) occur in Sub-Saharan Africa annually. The major factors that contribute to these deaths are:
· Severe bleeding
· Infections
· High blood pressure (eclampsia and pre-eclampsia)
· Complications from delivery
· Unsafe abortion
Fortunately, the global maternal mortality rate (MMR) is declining. The UN’s Sustainable Development Goals include a commitment (SDG3) to accelerating this decline still further. This will require a whole variety of interventions, but ensuring universal access to maternal health care services is an important part of this.
The Virtual Doctors charity is privileged to be able to assist Clinical Officers in Sub-Saharan Africa with their care of pregnant patients. We have Obstetric Specialist Volunteers both in the UK and in Zambia. They receive frequent requests for help about a whole range of issues affecting the pregnancy, labour and post-partum period. Their advice can be life-saving. They are often consulted about blood pressure problems in pregnancy; a previous Case from Malawi with helpful background information about pre-eclampsia, can be read on our website here. Below we report a further case; on this occasion the patient presented as an emergency with all the signs of this potentially life-threatening condition.
THE CASE
We were again contacted by one of the clinics we support in Malawi. A 32-year old lady had presented that evening in labour. She was 40-weeks pregnant. It was her third pregnancy and she had two healthy children at home. She had a raised blood pressure of 156/112mmHg and worryingly she also had symptoms and signs of severe pre-eclampsia with a headache, heavy proteinuria and significant peripheral oedema. The concern is that the condition can deteriorate and result in fitting (eclampsia); this puts the life of the mother and baby at risk.
Ukwe Health Centre in Malawi
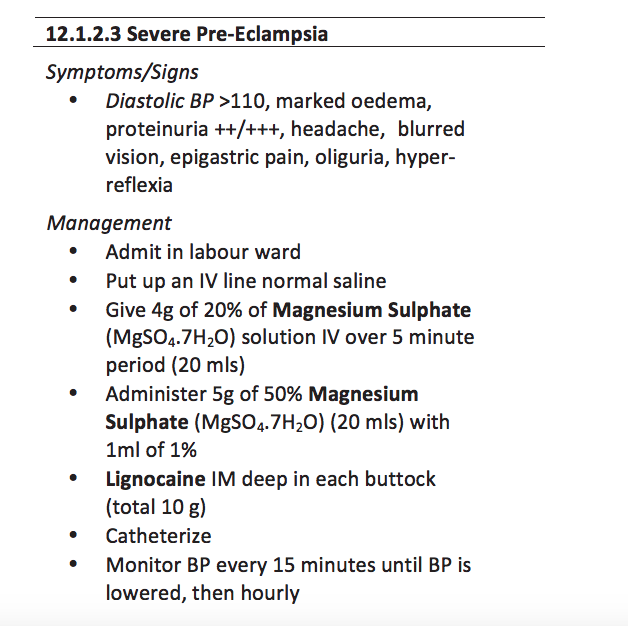
The Clinical Officer, George, had recognised that her presentation constituted a medical emergency. He had wisely followed local Guidelines (p259).
Taken from Malawi Standard Treatment Guidelines
He had admitted the patient and given her Magnesium sulphate as per protocol to try and prevent seizures (fits). He was monitoring the mother and the foetal heart rate. But because the patient was already in labour there was no time to refer her to a Hospital. So George turned to the Virtual Doctors for help.
One of our UK-based Obstetricians was able to give further advice about the duration of magnesium therapy and the choice and route of medication to lower her blood pressure. Guidance on the management of the labour was shared and recommendations were given on how to reduce the risks of bleeding post-delivery.
Clinical Officers complete comprehensive modules in Obstetrics during their training. They learn about normal pregnancy and antenatal care as well as pregnancy related problems. They need to be able to conduct a normal delivery by the end of their course and know how to deal with complications in labour. In a Rural Health Centre, they may often have to use these skills to assist expectant mothers. So they may become very experienced. But the equipment and monitoring they have available is only very basic. And they can feel quite isolated; the Virtual Doctors provide support in these stressful situations.
THE CASE CONTINUED
On reassessing the patient, the Clinical Officer confirmed that it was in fact a twin pregnancy. Multiple births are associated with higher risks to the mother and to the babies. And with the severe pre-eclampsia too, this was a precarious situation for all of them. The Volunteer reassured George that he had done all the right things so far.
At this point we just had to wait.
Later that night we were pleased to hear that the labour had successfully progressed to a twin delivery. The mother and her new son and daughter were said to be doing well! The Clinical Officer continued to monitor the mother’s blood pressure as per the advice he had been given and the magnesium was continued for 24-hours to prevent any fits post-partum. We understand that there were no further complications following the birth and that the family returned home after the period of observation was complete.
The Mother had been lucky to have received emergency treatment from George and his team; and he felt lucky that he’d been able to discuss this difficult case with an expert colleague.
There have been further cases where our team has given valuable advice about management of pregnancy induced hypertension, pre-eclampsia and even eclamptic fits. Each time the Volunteers try to share their knowledge and expertise, guiding and empowering the Clinical Officers, to ensure both the mother and the baby remain safe and well.
On a Global scale the impact of the Virtual Doctors may be small, but when we look at the individuals we have helped we can see the profound effects the Charity has.
FOLLOW UP
9 months later, the twins are doing well.