Buruli Ulcer
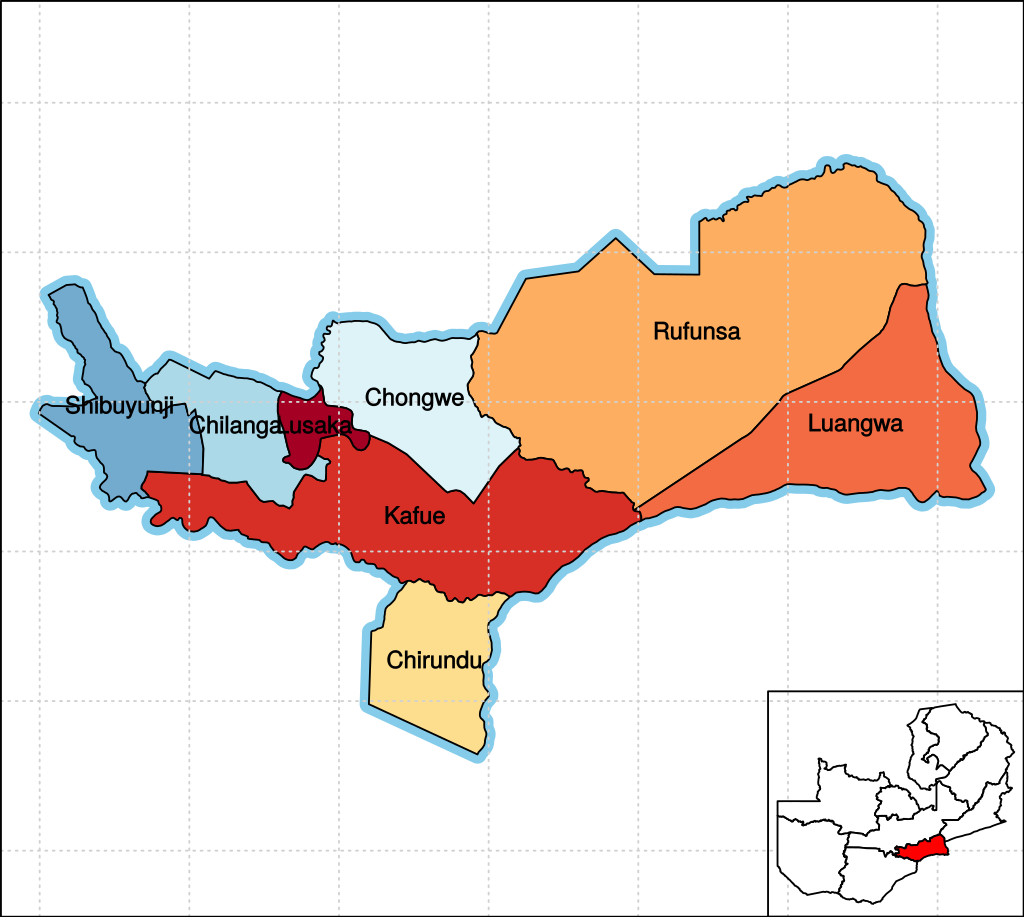
Our case this month comes from Chilanga District in Lusaka province.
Chilanga
Chilanga is located 20 km south of Zambia's capital city, Lusaka. It is located midway between Lusaka and Kafue on the Great North Road. Chilanga began as a suburb and constituency of Lusaka. Then, in 2011, The President of Zambia, The Late Michael Sata, made Chilanga its own town & district.
Chilanga District covers the area separating Lusaka from Shibuyunji District(west of Lusaka) as well as the area in between Lusaka and Kafue along The Great North Road, where its town centre is located. The Kafue Road (T2) runs through the center of Chilanga. Once a quiet and rarely used two lane road, it has now become a four lane and very busy road. A large volume of truck traffic moves through the town on a daily basis, including very large shipments traveling to the mines in the Copper Belt of Zambia. It is the main trunk road connecting Zambia with Zimbabwe through Chirundu and Victoria Falls via the T1 through Livingstone. North of Lusaka the T2 becomes The Great North Road connecting Southern Africa to Central and East Africa. Traveling away from the center of town, most of the land in Chilanga is used for sustenance agriculture. The areas away from the Great North Road are similar to most Zambian villages, with basic shelter for homes, and large Maize fields surrounding them. Because Chilanga is a transitional area between Lusaka Province and Southern Province, Zambia, both Tonga and Nyanja Bantu languages are spoken and understood, although, as with most of Zambia, many other tribal languages are also understood. English is the official language of Zambia, and most people in Chilanga can communicate in English.
The case this month comes from a patient at Chilanga Urban Health Centre which serves about 20,000 patients. The patient was a 24 year old woman who came to the health centre with 2 wounds on her upper left arm, near to where she had recently received a depo-provera (birth control) injection. They had been present for a month, and were being treated with antibiotics for bacterial infection/abscess. The Virtual Doctor agreed this was a likely diagnosis if there had been a painful abscess that had developed following the injection, which enlarged with a subsequent discharge of pus. This could result in open wounds secondary to abscess drainage. Given that there were 2 lesions without surrounding cellulitis and oedema, the doctor questioned whether these were simple abscesses and was concerned that a Buruli ulcer should be considered. Unlike an abscess, these may have started as a lump/nodule, and broken down to form an ulcer without significant discharge of pus, and usually without pain. He suggested, though assumed it might not be possible, a swab/biopsy of the base and microscope for acid fast bacilli or arrange a PCR blood test to confirm/exclude this. Otherwise the history was key to making the diagnosis. If the history was more suggestive of abscess, then continuing current treatment was appropriate. However, a Buruli ulcer would require different treatment. He advised that prompt use of antibiotics for these small lesions may be sufficient but should they get bigger surgical treatment would be advisable to prevent damage to bones/nerves/muscle. The antibiotics he suggested were rifampicin for 8 weeks, and streptomicin and clairthromycin for 4 weeks. Any worsening of the wounds would require urgent surgical treatment.
What is Buruli Ulcer?
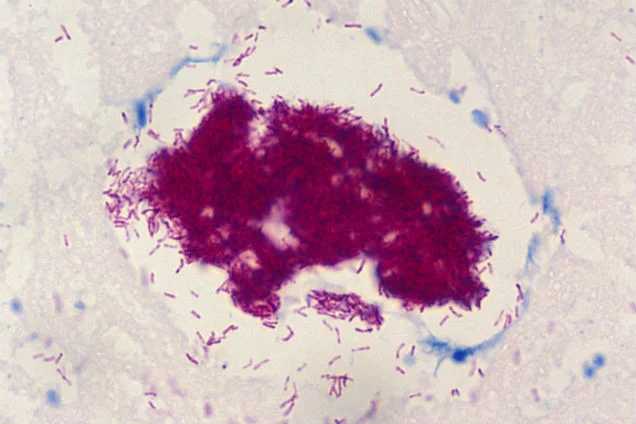
Buruli ulcer, caused by Mycobacterium ulcerans, is a chronic debilitating disease that mainly affects the skin. Through production of a locally active toxin, these ulcers can also result in destruction of soft tissue and bone. The organism belongs to the same family of bacteria that causes tuberculosis and leprosy, but M. ulcerans is an environmental bacterium and the mode of transmission to humans is as yet unknown. Because of this, prevention is currently impossible. Early diagnosis and treatment are crucial to minimizing morbidity and preventing long-term disability.
Photo credit: J. Buntine, WHO
Information about Buruli ulcer
Cases of Buruli ulcer have been reported in more than 30 countries worldwide. 10 years ago as many as 5000 cases were reported annually but this figure declined until 2016, when there were 1961.This then increased to 2713 cases in 2018.The increases and decline cannot be explained.
In Africa, Buruli Ulcers are seen in the Sub-Sahara. The WHO have received official reports of cases from West and Central Africa, including Benin, Cameroon, Côte d’Ivoire, Democratic Republic of the Congo, Nigeria and Ghana. There have been no confirmed cases of Buruli Ulcer in Zambia reported to the WHO.
Symptoms of Buruli Ulcer
Just over 50% of cases reported in Africa occur in adults, and 90% of lesions appear on limbs. Buruli ulcer often starts as a painless swelling (nodule). It can also initially present as a large painless area of induration (plaque) or a diffuse painless swelling of the legs, arms or face (oedema). Local immunosuppressive properties of the mycolactone toxin enable the disease to progress with no pain and fever. Without treatment or sometimes during antibiotics treatment, the nodule, plaque or oedema will ulcerate over days to weeks (usually 4 weeks) with the typical undermined borders. Occasionally, bone is affected causing gross deformities. They are usually painless, unless secondarily infected, although sometimes pain is experienced as lesions are treated and the toxin levels fall.
Treatment of Buruli Ulcer
Buruli ulcer can be cured with early detection and a combination of antibiotics. But, if diagnosed late, the condition can lead to permanent disfigurement and disability.
Information and statistics in this case come from WHO
https://www.who.int/news-room/fact-sheets/detail/buruli-ulcer-(mycobacterium-ulcerans-infection)
Disclaimer: This article is for information only and shouldn’t be used for diagnosis or treatment of medical conditions. If you have any concerns about your health consult a doctor or other health professional.