Cutaneous Larva Migrans
The Virtual Doctors Work
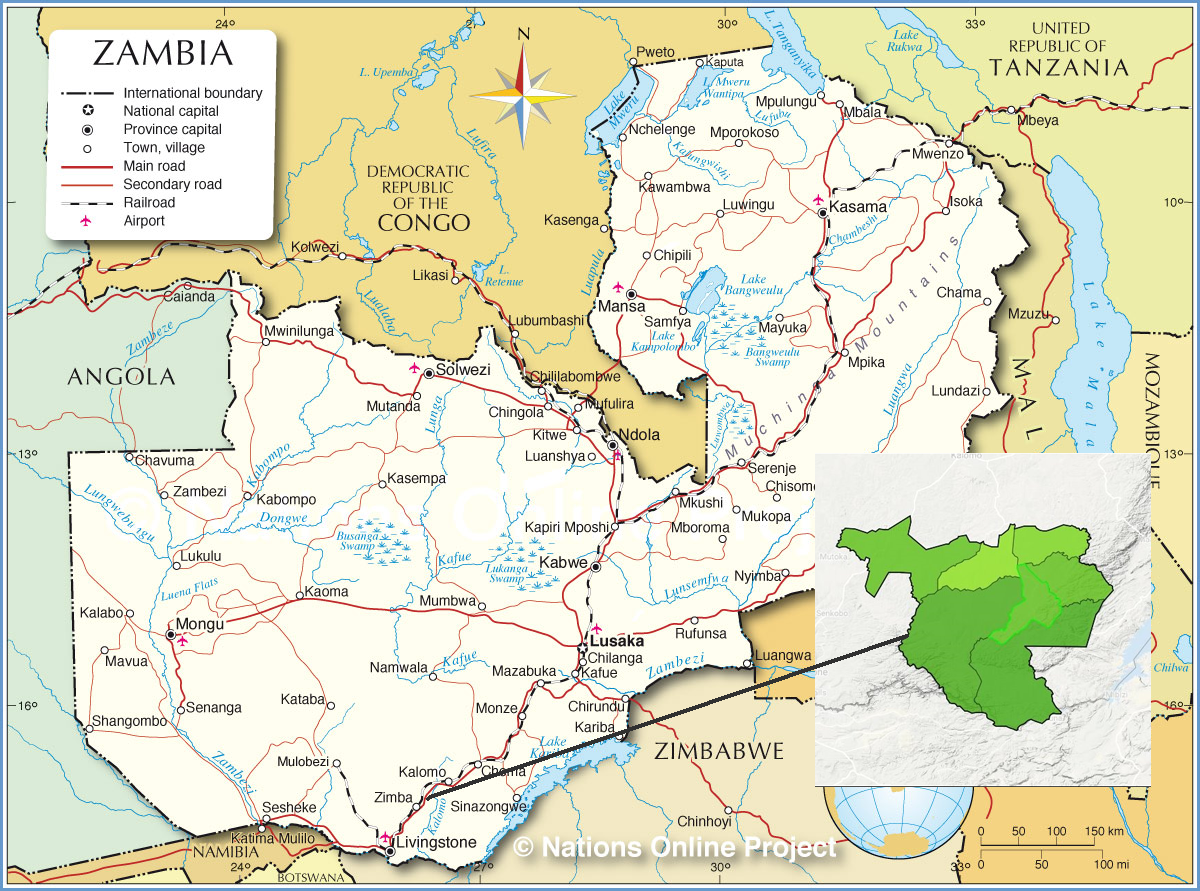
Exciting times for the Virtual Doctors. We have recently expanded so we can reach more Clinical Officers’ in Zambia. This means we are reaching further south in the southern province to cover Zimba and Kalomo districts. This month’s case comes from Simwatachela rural health clinic in the Zimba district.
So let’s travel down the river and explore a little of Zimba district.
Zimba with Simwatachela highlighted in bright green
Zimba is about 410km south-East of the capital Lusaka travelling on the Great North Road. Kalomo district, to which Zimba was a sub-district until 2012, lies on its northern border. Zimbabwe and the great Zambezi River lie to the south and east. Zimba district covers an area of 5000 sq km. Its population is approximately 67000 according to the 2010 consensus. Simwatachela covers 386 sq km and has a population of around 6000 but the population will have grown significantly since then.
Zimbo district is very rural with many villages and settlement –like farms. Agriculture is the main source of work from cattle rearing to crop production. The land supports maize, sunflowers, tobacco and groundnuts. All are dependent on good rainfall so its yield fluctuates.
Described as a Savanah woodland, Zimba is 1300m above sea level with dambo areas, pans and man-made dams. Dambos are complex shallow wetlands which are generally found in higher rainfall flat plateau areas. They usually flood during the rains and are especially important in maintaining the water table, so they are affectionately known as the ‘sponges’, retaining water throughout the dry season providing a much needed water supply and attract a wide variety of wildlife.
This is an example of a dambo in Kafue but they are similar across Zambia.
Zimba faces challenges in terms of infrastructure, housing and roads, but being close to Livingstone, the tourism capital of Zambia, there is great potential for tourism to development in this area. There are protected areas too including the Zimba Hills Local Forest and idyllic beach locations along the Zambezi perfect to attract the adventurous and curious. The Zimba hills local forest covers an area of 18800 hectares and is about 40km south west of Zimba town.
Virtual Doctors support 10 Rural Health Centres, the Zimba mission hospital and Zimba’s district health office in Zimba District
One of the many patients to visit Simwatachela Rural health centre this month was a mother with her 10 month baby boy. Seven days ago she had noticed a raised area like a worm under his skin which moves and grows. It was very itchy and there were multiple sores. The Clinical Officer could see pus coming from the wound and a visible head of a worm. He sent the volunteer doctor a helpful picture and wanted to know what to do next. Amazingly there was a similar case seen in the Naluja RHC in Kalomo district.
The case in Simwatachela
The case in Naluja
Our GP volunteer doctor replied remarking how he had seen a simiar case from Naluja the same week. He felt this was probably Larva migrans (a hookworm infection) or Larva currens (a threadworm infection) and advised treatment with mebendazole or albendazole for 3 days. He was also going to get an opinion from a skin specialist to make sure we had the right diagnosis.
What is Cutaneous Larva Migrans?
Cutaneous Larva migrans is a parasitic skin infection in humans caused by various nematode parasites of the hookworm family (Ancylostomatidae). Humans are incidental hosts of this parasite which normally live in dogs, cats and wild animals and should not be confused with other members of the hookworm family for which humans are definitive hosts! Namely Ancylostoma duodenale and Necator americanus. But sometimes humans become infected with the hook worm larvae by walking barefoot on a beach, or by contact with soil contaminated with animal faeces.
The larvae that come into contact with the skin can penetrate through hair follicles or tiny skin cracks and then migrate under the skin. They can’t penetrate the dermis (the thick layer of skin under the epidermis which contains the blood vessels and nerves) in humans so remain in the outer layers of skin of the human and cannot complete their life cycle.
How does it present?
The most common areas of hookworm penetration are feet, hands, knees, abdomen and buttocks. There is sometimes a non-specific red area at the site of entry of the larvae. It can remain dormant for months or start migrating straight away. When this happens raised pink, or flesh-coloured tortuous snake like tracts that are2-3mm wide form. This is caused by an allergic immune response to the larvae or its by-products.
Tracts can advance between 2mm-2cm a day. These skin lesions are intensely itchy, causing the patient to scratch resulting in sores as we can see in the pictures above.
How do we treat it?
Cutaneous Larva migrans is usually a self-limiting but can be treated with albendazole or ivermectin (antihelmintic drugs). Most cases will resolve within 4-8 weeks as the larvae cannot reproduce so eventually die.
Antihistamines and topical corticosteroids can help to treat the itch.
Complications
Secondary skin infection, as seen in our cases, may need treating with antibiotics.
Löfflers disease. This can occur if there is a heavy infestation of larvae and is a combination of pulmonary (lung) infiltrates and eosinophilia.
Skin conditions are a large part of the work at Virtual Doctors and we are able to view great photos of these conditions sent by the Clinical Officers. If there are any skin specialists out there who read this blog and fancy joining the team please contact us!
Disclaimer: This article is for information only and shouldn’t be used for diagnosis or treatment of medical conditions. If you have any concerns about your health consult a doctor or other health professional.