Sickle Cell Crisis
Virtual Doctors Work
This month our case comes from the Chongwe district found in the Lusaka province of Zambia. This district covers an area of 8669 square km, with a population of just under 250,000. It encompasses most of the lower Zambezi national park, an unspoilt area of wilderness. It sits on the Zambezi flood plain ringed by mountains. Chongwe is especially famous for its elephants which feed mostly on the winter acacia trees. The river not only supports the population but countless animal species too. This is a popular tourist area for adventurers.
Within Chongwe district we support 2 rural health centre and the district hospital.
Chongwe
Chongwe
Early in January 2017 a 2 year old boy was brought into Chongwe hospital by his mother. He was extremely unwell. He was known to have a condition called Sickle cell Disease. For the last 3 days his mother said he had fevers, swelling of his joints, cough, difficulty breathing, runny nose, diarrhoea, vomiting and poor appetite. He was on medication to prevent him from getting malaria (deltaprim) and folic acid to prevent him becoming anaemic (a complication of his underlying condition). In his report to the Virtual doctors (VDrs), the clinical officer (CO) said the child looked ill with swollen joints and high fever. He had been started on an intravenous antibiotic, pain relief and a drip of fluid to treat dehydration. The clinical officer was concerned the boy was having a sickle cell crisis. Helpfully blood results were also sent showing the child to be severely anaemic (very low number of red blood cells). The Virtual Doctor agreed thinking the crisis was likely to have been triggered by a chest infection. She was, however, concerned that other diagnosis were considered, particularly malaria, to ensure the child was treated correctly.
After some more discussion The Virtual Doctor confirmed that the patient was receiving the right treatment and gave the CO more information to help manage the very ill patient and what to do if the patient's condition changed. The CO was working hard to look after this patient. During the day he updated the VDr with the good news that the patient was indeed improving and a few days later was well on the way to a full recovery.
What is Sickle Cell Disease?
Sickle cell disease (SCD) is a group of serious, inherited conditions which affects the blood and various organs of the body. It affects the red blood cells, which contain a special protein called haemoglobin which carries oxygen from the lungs to all parts of the body. People with SCD have sickle haemoglobin which is different from normal haemoglobin. When a sickle haemoglobin gives up its oxygen it sticks together inside the red blood cell making the cells rigid and sickle shaped (like a crescent moon) as can be seen in the picture below:
Because of their shape they can't squeeze through small blood vessels and block them stopping oxygen from reaching the places where it’s needed. This can lead to severe pain and organ damage. The sickling can happen suddenly causing symptoms which are known as a sickle cell crisis (as with our patient). Some conditions can trigger this such as a cold, infection or lack of body fluid (dehydration).
The red cells containing sickle haemoglobin also do not live as long as normal red blood cells leaving the person with a moderate and persistent anaemia. In between episodes of illness people with SCD generally feel well.
Who gets Sickle cell?
SCD is inherited. Two genes, one from each parent containing the information for sickle haemoglobin, is needed to have the disorder. If you only inherit one of these genes then you will have sickle cell trait which is much milder. Sickle cell trait does give the carrier some protection against malaria.
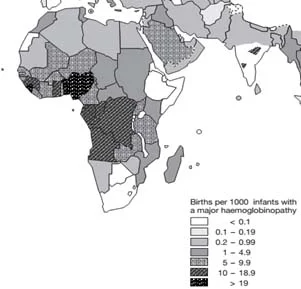
SCD and the different traits are mainly found in people whose family origins are African, Afro-Caribbean, Asian or Mediterranean. On average 1 in 2400 babies born in UK have SCD. In Zambia exact figures are hard to find, however, the world Health Organisation puts the figure between 5 -9.9 per 1000 births (for all the haemoglobin disorders) as seen on this map below: Sickle cell trait is thought to affect approximately 18% of the general Zambian population.
Global distribution of haemoglobin disorders in terms of births of affected infants per 1000 births
How Does SCD Present?
SCD can begin to cause problems between 3 and 6 months of age. The symptoms include anaemia, poor growth and increased susceptibility to infection. People with SCD are more prone to certain types of germ (bacteria) which cause pneumonia, meningitis, septicaemia or bone infections. (The usual culprits being pneumococcal, H.influenza type b and meningococcal). These infections can be life threatening particularly in the under 5 year age group. It is estimated that every day 500 children with SCD die in Africa and Asia due to overwhelming pneumococcal sepsis (overwhelming infection), malaria or unrecognised splenic sequestration (which occurs when a lot of sickled red cells get caught in the spleen causing severe pain and a sudden drop in haemoglobin).
Living with SCD
Symptoms of SCD come and go. There is a lot of individual variation in symptoms too. Some people are affected frequently and others rarely. Problems include episodes of pain, infections, acute chest syndrome where there are blocked blood vessels in the lungs and episodes of anaemia. Most organs can be affected.
Managing SCD
The treatment of SCD is a developing area of medicine.
Patients with SCD should be given a daily antibiotic to prevent infection (penicillin) particularly important in the vulnerable under 5s.
Immunisations of all the usual childhood vaccines plus meningitis and hepatitis B and flu vaccine are highly recommended in all age groups. Folic acid supplements are given to help the body make new red blood cells.
In malarial areas it is important to take malaria protection medication and avoid mosquito bites.
To keep healthy it is recommended to keep well hydrated, regular exercise but avoid over exertion .It is important to keep warm.
Any signs of infection should be treated quickly.
Hyrdoxyurea taken regularly can help reduce the number of painful crises caused by the disease and to reduce the number of blood transfusions. It does require regular monitoring with blood tests due to its possible side effects. It was first used in chemotherapy.
Cure is only possible with a bone marrow transplant to replace the faulty stem cells which produce haemoglobin.
Sickle cell crisis
Treat with painkillers, hydration by mouth if possible but intravenous fluids if not, oxygen and antibiotics.
The Future
Currently the high number of deaths due to SCD in Africa and Asia are in the under 5 age group, often before diagnosis has been made. In the UK babies are tested at 5 days for SCD and other conditions. A blood spot is taken from a heel prick. Babies in the USA are also screened.
This is not the case in Africa, however, some countries are trying to address this. In Uganda for example they are considering the steps to make a national sickle cell program by building on the existing HIV program using dried blood spots. So exciting times in tackling non-communicable diseases.
Disclaimer: This article is for information only and shouldn’t be used for diagnosis or treatment of medical conditions. If you have any concerns about your health consult a doctor or other health professional.