Martin Dedicoat: On the Frontline of the COVID-19 Response
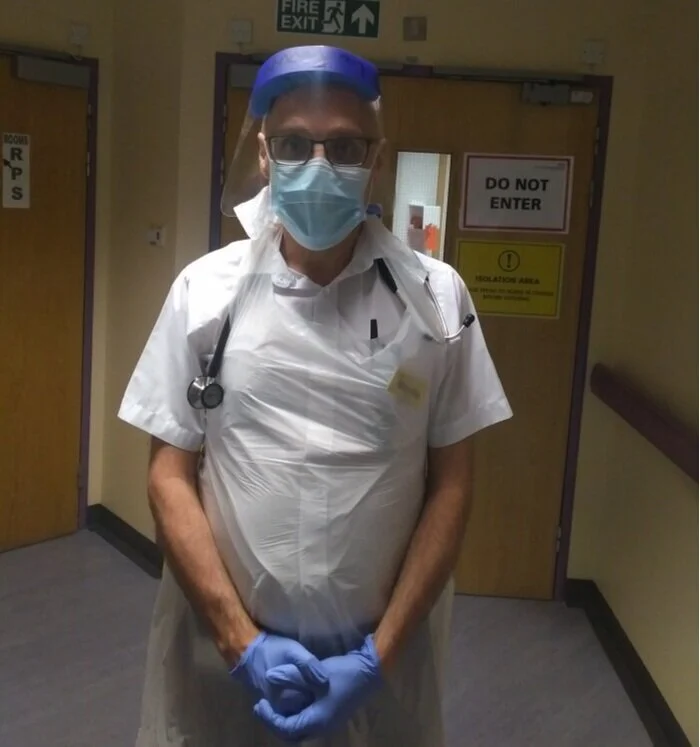
Dr. Martin Dedicoat is a consultant in infectious diseases at Queen Elizabeth Hospital Birmingham and also one of our Virtual Doctors. We interviewed him as part of our #PassTheMic campaign.
He is currently TB clinical lead for Birmingham and Solihull. He trained in London, Birmingham, Ecuador and South Africa.
Martin was working at the hospital in Birmingham throughout the first wave of the COVID-19 pandemic, where the work of every single member of staff was invaluable. We caught up with Martin during the summer to find out about his frontline experience on the wards.
Preparing for Patients
Martin came back from leave just as the hospital was preparing for an influx of COVID-19 patients. Beds were being emptied, patients discharged and COVID wards planned, but nobody was quite ready for the whirlwind that was about to hit.
The first step was freeing up as many beds as possible. Martin says, ‘suddenly we basically had to discharge the patients, no one was forced to go home obviously but people went home pretty quickly’. Once you realise that the hospital might not be the safest place to be, due to the imminent pandemic, being treated at home certainly seems the preferred option. For a brief period the hospital was then largely empty, a very eerie feeling for the staff on the wards who are used to working in one of the UK’s busiest hospitals. ‘I've worked at this hospital on and off since 1996 and I've never ever known it to have more than one or two beds empty, it’s usually people waiting for beds – but we had wards of empty beds.’ And then, overnight, the tide of patients started to arrive. COVID-19 had arrived in Birmingham and every doctor, nurse and member of staff was in for months of very hard work.
Becoming a COVID Hospital
The hospital became a COVID hospital immediately and, Martin tells us, the response from the staff was unfaultable. They got on with everything that needed doing, regardless of whether they liked it or not, and everyone switched their focus to fighting the disease. Outpatient physicians were drafted in to work on the wards and a new 4x4x4 rota was put in place. Staff worked four days in a row then four nights in a row, then had four days off. This system worked well and ran smoothly and, Martin says, ‘the intensive care doctors in particular worked incredibly hard.’
Martin’s infectious diseases ward became a pre-intensive care ward. Any seriously ill patients that arrived at the hospital and were not palliated, were taken to Martin’s ward. From there the majority of them were then later moved to intensive care. Martin told us ‘intensive care at Birmingham is used to treating 10-15 patients on average, but during the peak of the pandemic they were up to 35 patients.’ The staff worked incredibly hard to treat over double the number of patients they would usually be seeing to.
Pushing the Limits
When treating and interacting with the patients, Martin was shocked by just how many were seriously ill with the disease. Furthermore, many of them didn’t seem to realise just how serious their condition was. This was the striking difference between coronavirus and the flu. Martin says, ‘the flu is a more systemic disease so you feel really dreadful. With COVID, we found that some of the patients looked quite well, but their lungs just simply were not working.’
Trying to treat these seriously ill patients pushed the hospital’s resources to the limit. The amount of oxygen doctors can usually deliver on the ward is about 24 to 28%. Just to keep COVID patients stable, they were having to deliver up to 98% oxygen. This inevitably led to oxygen shortages. Martin explained ‘I know that there’s a lot of oxygen in the atmosphere, but we’ve got to distill it into tanks and share it around. The pressure was dropping in the tubes, which is not something that the hospital was designed for, this is basically a once in 1,000-year event. It was frightening.’
Martin tells us that there were nights when doctors had to go through the wards and turn down oxygen levels very slightly. They were trying to save just a liter from each patient to ensure the pressure across the hospital didn’t drop. Fortunately, it didn’t.
The work at Birmingham hospital went on in this way for just over a month before the pressures and numbers of patients started to ease off. The hospital staff have all done an incredible job to maximize resources, deliver excellent patient care and see the city through a very challenging first wave of COVID-19.
It is very interesting to hear about Martin’s experience on the frontline and get an insight into just what our medical staff are dealing with every day when fighting this relentless pandemic.